US Secretary of State Antony Blinken Visit
US Secretary of State Antony Blinken during his visit to the Nigerian Institute of Medical Research Lagos. From left, Professor Oliver Ezechi, Director of Research (representative of DG, Prof. Babatunde Lawal Salako).
Others are Dr. Joseph Shaibu (Researcher and Innovator) Dr. David Oladele (Head , Clinical Sciences Department), Professor Rosemary Audu (Head, Department of Microbiology), Dr. Muinah Fowora (Researcher and Innovator) and Chika Onwuamah (Researcher and Innovator)
National Malaria Elimination Programme (NMEP) Visit
On the 11th of January 2024, the DG-NIMR hosted the delegates from National Malaria Elimination Programme (NMEP) lead by Dr Nelson and SC Johnson on a visit to evaluate their Insectary in NIMR.
The essence of the visit is to plan is to renovate and upgrade Insectary so as to support more research collaboration between the two organizations.


Adewunmi Desalu Parkinson’s Foundation Visit
Nigerian Institute of Medical Research aims to collaborate with Adewunmi Desalu Parkinson’s Foundation to undertake research that will improve public health in Nigeria and sub-Saharan Africa.
Below are pictures of the DG-NIMR signing the memorandum of understanding on behalf of the institute along with Ms. Laura Ede, the Executive Director Adewunmi Desalu Parkinson’s Foundation on 16th of January 2024.



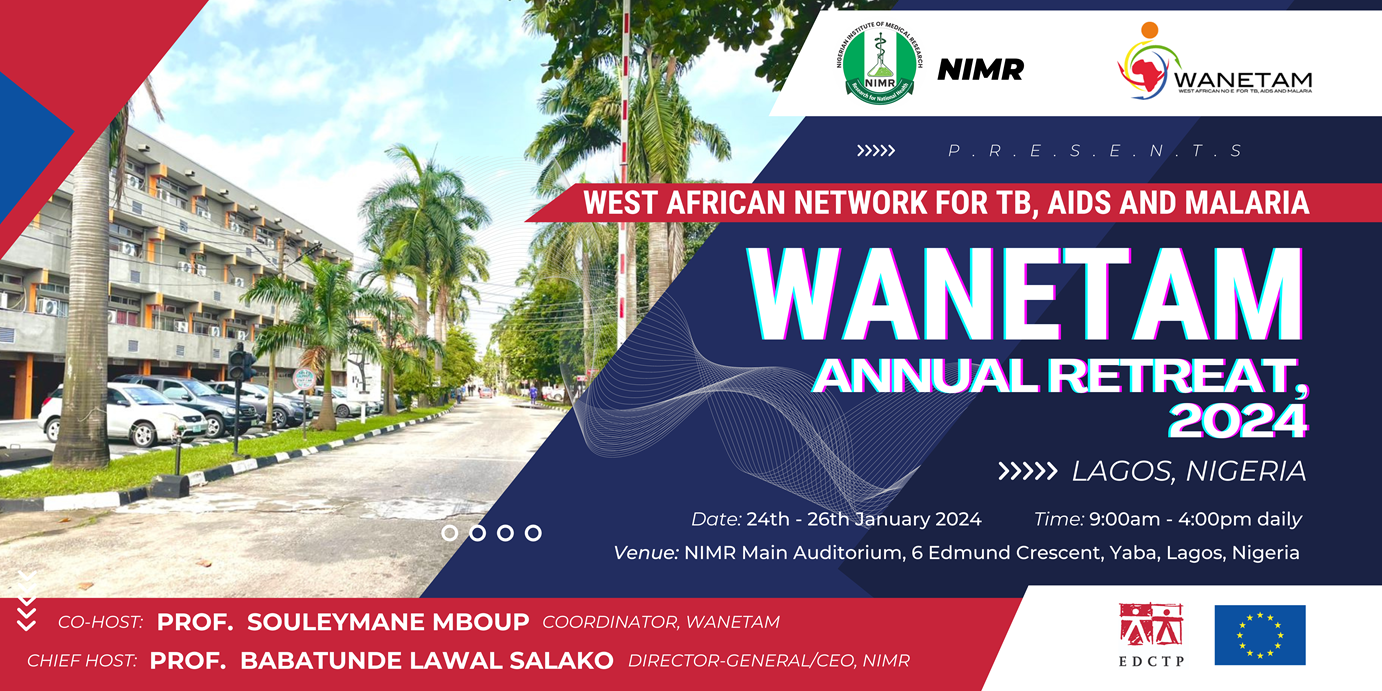
WANETAM Annual Retreat 2024
Africa remains burdened by the high mortality related to poverty-related diseases such as HIV, Tuberculosis, Malaria, and other Neglected Tropical Diseases. Recognising these challenges and the need to proffer sustainable solutions for the sub-region, the West African Network for Tuberculosis, AIDS, and Malaria (WANETAM) was established in July 2009. WANETAM is one of the Networks of Excellence supported by the European and Developing Countries Clinical Trials Partnership (EDCTP). The network has grown since inception to a membership of 25 institutions from 12 West African countries and 5 institutions from 4 European countries.
The main goal of WANETAM is to build regional, national, institutional, and individual capacities to conduct research including clinical trials. WANETAM conducts its strategic goals under the following work packages (WP); WP1- Tuberculosis; WP2- Malaria; WP3- HIV; WP4- NTD/EBOLA; WP5- Cross cutting trainings and Project management. Kindly visit the website http//www.wanetam.net.